Abstract

Background: Sickle cell disease in pregnancy accounts for 0.14-0.2% of pregnant women seen in Antenatal clinic in Niger Delta Nigeria.1,2Chronic anemia in SCD during pregnancy could lead to a cascade of maternal and fetal complications. The aim of this study is to assess the various types of ABO blood groups of pregnant SCD women at booking and the severity of anemia. The outcome of this study will help in making recommendations of ABO blood types most suitable to improve the quality of life of SCD patients. This may contribute to guidelines for safe blood transfusion in SCD.
Methodology: This was a-ten-year retrospective study of all registered SCD pregnant women seen at the antenatal clinic of Braithwaite Memorial Specialist Hospital (BMSH) Port Harcourt (January 2004- December 2013). Data on gestational age, Hemoglobin (Hb) electrophoretic pattern, Hb concentration and blood group were obtained at booking clinic. Data were analysed using Epi-info version 7.02 by WHO, Geneva Switzerland and CDC, USA.
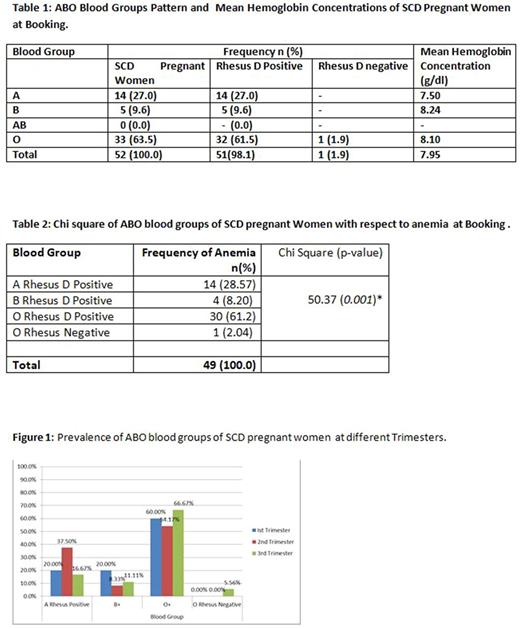
Result: A total of 52 Hb SS pregnant women were seen during the study period. The average booking trimester was the 2nd trimester. 94.2 % (49) were anemic (<11.0 g/dl)3 while 5.8% (3) were non anemic (≥ 11 g/dl). 27.0%, 9.6% and 61.5% were A, B and O rhesus D positive blood groups respectively. No AB blood group was recorded from this study [Table 1]. The O rhesus D positive blood group was significantly more prone to anemia [30 (61.2%)] than other ABO blood groups (X2=50.37; 0.001) [Table 2]. 20% (1/5) of B rhesus D positive and 6.3% (2/32) of O rhesus D positive patients were non-anemic. All A rhesus D positive blood were anemic. The highest prevalence of A rhesus D positive blood group (37.5%) was in 2nd trimester, that of B (20%) and O (66.7%) rhesus D positive blood groups were in 1st and 3rd trimesters respectively [Figure 1].
Conclusion: Although most SCD pregnant women in this region are O rhesus D positive blood groups, B rhesus D positive blood group patients appear to be less susceptible to anemia. There is need to carry out more elaborate study on this group of blood.
References
Ugboma HA, George IO. Sickle cell disease in pregnancy: Maternal and fetal outcome in Port Harcourt, Nigeria. Br J Med Med Res 2015;7:40-4.
Nwabuko OC, Okoh DA, Iyalla C, Omunakwe H. Prevalence of sickle cell disease among pregnant women in a tertiary health center in south-south Nigeria. Sub-Saharan Afr J Med 2016;3:132-6.
World Health Organization. The Prevalence of Anemia in Women: A tabulation of Available Information. WHO/MCH/MSM/92.2. Geneva, Switzerland:WHO;1992.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal